Dentures: Affordable & Comfortable Solutions
Tooth loss is far more than a cosmetic concern—it fundamentally affects chewing efficiency, speech articulation, and the structural integrity of the jaw-bone. When teeth are missing, the supporting alveolar ridge begins to remodel and resorb, compromising the bite and altering facial contours. At the same time, many patients believe dentures are only a cosmetic fix; in reality, untreated edentulism (complete tooth loss) can lead to nutritional reduction, changes in phonetics, and even progression of adjacent periodontal disease. According to the patient-educational material provided by the practice, missing teeth interfere with everyday activities like eating and speaking—not just the way one looks.
Consequently, the decision to replace missing teeth with a well-designed denture is not simply aesthetic—it is restorative and functional. The following sections will explore the causes of tooth loss, the range of denture options, the material science behind them, the benefits and drawbacks, and the necessary maintenance for long-term success.
Causes
The primary triggers for tooth loss include advanced caries, trauma, and especially periodontitis—a condition wherein plaque-induced inflammation leads to loss of the periodontal ligament and alveolar bone. As teeth are lost, the jawbone no longer receives normal mechanical stimulus from biting and chewing, and begins to atrophy (bone resorption). Over time this can cause the residual ridge to flatten, making future prosthetic retention more challenging.
The practice’s blog touches on how missing teeth impact more than appearance: chewing becomes difficult, speech can become slurred, and facial support diminishes—leading to a “sunken” appearance around the lower third of the face. Beyond appearance and function, untreated gaps can allow adjacent teeth to drift or tilt, create uneven occlusal forces, and potentially contribute to temporomandibular joint (TMJ) stress. Thus, the placement of an appropriate denture—or denture alternative—serves multiple clinical goals: restore function, prevent further damage, and safeguard overall oral health.
Treatment Options or Product Comparisons
When considering replacement of multiple or all missing teeth, patients generally encounter a spectrum of options:
- Conventional removable full or partial dentures: These are removable prostheses that replace an entire arch (full denture) or several missing teeth while retaining some natural teeth (partial denture). The blog emphasises these as affordable and comfortable solutions.
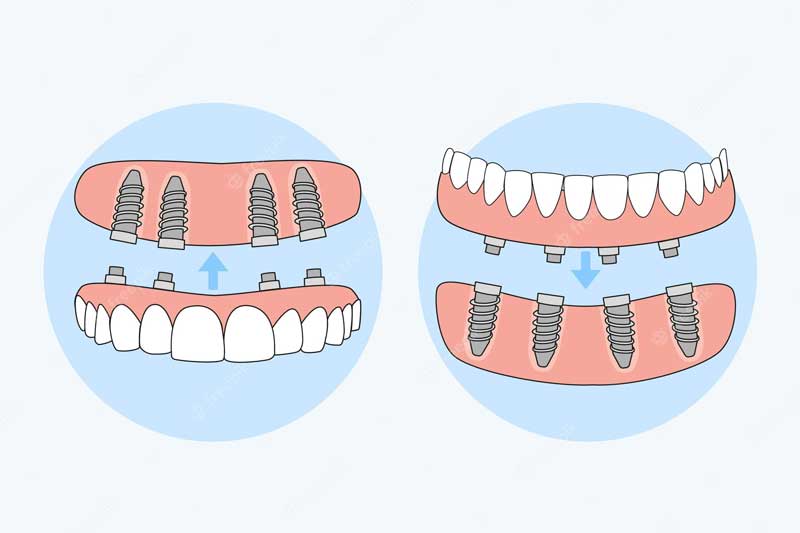
- Implant-retained dentures (overdentures): These prostheses are anchored onto endosseous implants (typically titanium) that serve as artificial roots. The greater retention affords improved chewing efficiency and stability. The blog mentions that for patients seeking more stability, implant anchorage is available.
- Fixed implant-supported full-arch bridges: In cases where cost and surgery are acceptable, a fixed prosthesis (for example, an “All-on-4” style) can be provided, which offers near‑natural stability and function.
In terms of cost and complexity: conventional dentures represent the least invasive, lowest‑cost option. Implant-supported options come at higher cost and require surgical healing time, but deliver significantly enhanced retention and bone-preservation benefits. According to the practice, their goal is to deliver “affordable and comfortable” solutions tailored to each patient’s needs and budget. Thus, the selection of denture type depends on the patient’s oral anatomy (bone volume, ridge shape), systemic health (healing capacity, bone metabolism), financial investment and functional/lifestyle goals.
Technical Details
Modern denture fabrication begins with a detailed clinical examination and diagnostic imaging (including digital scans, 3D imaging or intra-oral scanning). The practice mentions that digital impressions and advanced technology are part of their workflow.
For removable dentures:
- The base is typically constructed of acrylic resin (polymethyl methacrylate, PMMA) that adapts to the soft-tissue ridge and supports the prosthetic.
- The denture teeth may be acrylic or, in premium cases, porcelain or composite resin; each material has trade-offs in wear resistance, aesthetics and cost.
- Fit and occlusion are critical: establishing proper vertical dimension of occlusion (VDO), centric relation, and balanced occlusal contacts ensures optimal function and comfort.
For implant-retained systems: Titanium implants are placed into the alveolar bone and allowed to osseointegrate (bone fuses with the implant). After healing, either locator attachments, bar/clip systems or fixed frameworks support the prosthesis. The blog refers to such implant options for patients desiring greater retention.
At delivery, multiple try-in visits ensure proper fit, aesthetics, bite and comfort. Soft liners or flap relief adjustments may be used especially when residual ridges display change or sensitivity. From a material-science standpoint, acrylic/PMMA offers flexibility, ease of repair and low cost, but is less wear-resistant than porcelain teeth and may require more frequent relining if ridge resorption occurs. Implant systems, by contrast, help preserve local bone and produce superior retention, albeit at higher expense and requiring more technical treatment planning.
Benefits & Advantages
There are several important clinical and patient-centred benefits to well-fabricated dentures. First and foremost, they restore masticatory (chewing) function—enabling a more diverse diet, better nutrition and improved general health. The practice states that their dentures restore not just “a smile” but comfort, confidence and function.
Second, speech clarity is often improved once missing teeth and supporting structures are replaced, especially when phonetic deficiencies were present because of gaps or soft-tissue collapse. Third, facial support and aesthetics improve: by restoring the missing tooth-bearing ridge and prosthetic replacement of teeth and gums, the lower face can appear fuller and less collapsed. Fourth, cost-effective dentures (particularly the removable variety) allow many more patients access to tooth-replacement treatment than more expensive options might.
Last, when digital workflows and modern techniques are used (as mentioned by the practice) the fit and comfort of dentures have improved substantially compared to older-generation prostheses. This improves patient satisfaction and long-term compliance.
Considerations
It is essential to be candid about the limitations. Removable dentures seldom match the chewing efficiency or proprioceptive feedback (sensory input) of natural teeth or implant-retained teeth. Some patients may experience discomfort, sore spots, reduced bite force, or instability—especially if the residual ridge is severely resorbed. The practice’s blog underscores that candidacy evaluation is important.
Residual bone resorption continues under a removable denture, meaning periodic relines or replacements may be necessary. The blog indicates affordability but also emphasizes ongoing professional care. Patients with poor dexterity, uncontrolled systemic disease (e.g., uncontrolled diabetes, smoking) or severely compromised ridges may be better suited to implant options—or may require preparatory treatments. Implant-retained dentures, while superior in many respects, involve surgery, healing periods and higher cost; they require sufficient bone volume and healthy systemic conditions for osseointegration.
Therefore, every patient must be evaluated individually: ridge anatomy, oral hygiene capacity, systemic health, financial considerations, lifestyle expectations, and long-term maintenance willingness all factor into the choice.
Long-Term Outcomes
Proper maintenance is the key to long-term success. For the removable prosthesis, daily cleaning is vital: brushing the denture with a soft-bristle brush and non-abrasive cleaner, soaking overnight in a denture-cleaning solution, and storing properly to avoid warping. The blog refers to the practice’s instructions on brushing, soaking and storing dentures to avoid staining and deformation.
Regular dental visits enable the dentist to check for tissue changes, reline or rebase the denture if needed and address any sore spots or occlusal imbalance. Many sources suggest the functional lifespan of a high-quality denture is about five to ten years, depending on wear, change in tissue contours and patient factors. In implant-supported cases, maintenance includes evaluating peri-implant soft tissue health, checking attachment wear (e.g., locator retention components), and tracking implant stability.
With conscientious care, either removable or implant-retained dentures can provide durable and highly satisfactory functional outcomes, restoring confidence in eating, speaking and smiling.
Recap of Essential Points
Tooth loss has wide-reaching consequences, encompassing function, speech, facial structure and overall oral health. Dentures remain a viable and affordable replacement option, especially when fabric- created using advanced materials and digital workflows, and when properly maintained. The treatment range—from conventional removable to implant-support—offers different trade-offs between cost, complexity, stability and long-term outcomes. Patients must assess their candidacy and choose with realistic expectations. Regardless of choice, the role of a skilled dental team in diagnosis, planning, fabrication and follow-up remains indispensable.
For those seeking a comfortable, affordable denture solution, call (407) 777-2071 to schedule a consultation.
